Sexually Transmitted Infections
The Hawkes Bay region has higher than average population case rates of sexually transmitted infections
Young people in Hawkes Bay and nearby Tairāwhiti, MidCentral and Whanganui DHB regions have some of the highest rates of bacterial sexually transmitted infections (STIs) in New Zealand. STIs like chlamydia and gonorrhoea are one of the main preventable causes of ill-health among young New Zealanders.
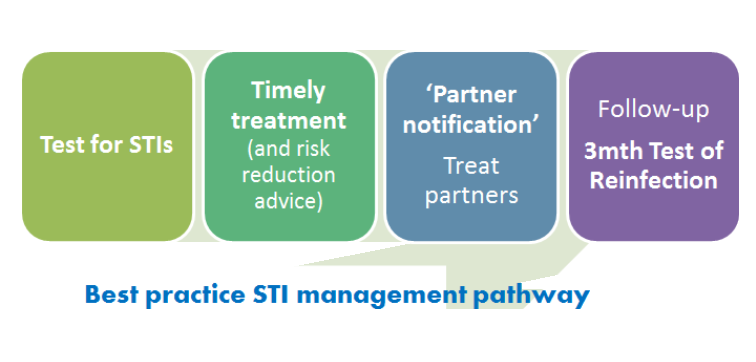
Good clinical management of bacterial STIs is one of the cornerstones of STI control. Routinely addressing all steps in the best practice STI management pathway helps to reduce complications at an individual level, identifies asymptomatic cases and reduces the spread and consequences of STIs in the community.
Reinfection following treatment for chlamydia or gonorrhoea is common – often because sexual partners/contacts have not been treated. The risk of long-term complications such as infertility is greater following reinfection, so testing for reinfection is recommended three after treatment.
Study aims
- We aimed to gain an understanding of factors impacting on the provision of sexual health care in four regions of New Zealand with higher than average rates of STIs.
- We also aimed to assess the extent to which guideline recommendations regarding testing for reinfection are being met, and to determine what proportion of annual chlamydia and gonorrhoea diagnoses are repeat or re-infections.
a. Issues impacting on sexual health and the provision of sexual health care
We interviewed 22 local clinicians to gain insight into some of the challenges facing the sector and to identify any ideas they had on how to strengthen the delivery of good sexual healthcare. Interviewees worked in a range of services including general practice, youth health, Family Planning, Sexual health and Maori-provider clinics. Ten of our interviewees came from the Hawkes Bay, and four from each of the other three DHB regions.
Key findings: Insights from local clinicians
We heard from many participants that declining, lack of, and ever-changing models of funding for sexual health care is a major challenge that has significant implications for the provision of, and access to quality sexual health care.
A wide range of societal issues were also identified as having an impact on sexual health outcomes (e.g. drugs and alcohol, mental health, stigma, sexual violence, bullying, poverty, racism, lack of social connectedness, cultural taboos, peer pressure, dating apps, social media, inadequate school-based sexual and reproductive health education).
While many of the issues reported by participants were common across all the regions, some regions face unique challenges related to population demographics and employment. For example seasonal workers, forestry workers, students and other transient groups can be hard to reach for healthcare, and can be challenging to follow-up for treatment, and partner notification. Consultation costs for sexual healthcare vary within and between regions, with some services offering free consultations regardless of age, others offer reduced consultation fees for young people but with variable upper age limits across services.
Consultation time constraints, high staff turnover, restructuring of services and gaps in provider’s knowledge of STI management were cited as challenges faced in the provision of good sexual health care. Better access to clinician education and ongoing sexual health updates, more collaboration across services, removing access barriers for patients, normalising conversations about sexual health in consultations and reaching people outside of clinical settings for testing were suggested as ways forward. Some excellent initiatives have been implemented in some clinics to prioritise patient access, for example offering free appointments for sexual healthcare, after hours appointments, outreach clinics, upskilling nurses, reducing missed opportunities for STI testing and offering express self-testing options.
b. Patterns of STI testing, retesting and reinfection

To determine how often testing for reinfection occurs, we analysed anonymised testing data from the two laboratories providing diagnostic services for our four DHB regions. We identified ‘first tests’ in the dataset over a two and a half year period (2015-2017) then tracked individuals in the data (using unique lab-assigned numbers) to see if they received a subsequent test within six months, and if so, what the outcome of that test was.
Key findings
Females made up the clear majority of those receiving testing for chlamydia and gonorrhoea (82%). Reinfections accounted for 21% of all cases diagnosed in 2017. That is, one fifth of all cases diagnosed in 2017 were in individuals who had already had a positive chlamydia or gonorrhoea test that year.
One third of individuals were retested within the recommended 6-month period (34%) and one in five of those retested were positive on retesting (21%). Clear differences were observed in retesting and reinfection outcomes by sex, age and ethnicity. Males not only had very low rates of initial testing, but also retesting. Females were nearly two times more likely to be retested than males, people of European ethnicities and those aged 15-19 years old were also more likely to be retested. When retested, females, 25-29 year olds, and European were more likely to be free of infection.
Conclusions
While many important factors impacting on sexual health and wellbeing are beyond the control of primary care providers, there are many dedicated individuals working tirelessly within a system that doesn’t always meet the needs of patients. There is a clear need for greater focus on the management of STIs – beyond simply testing and treating at an individual level if we are to reduce the community prevalence of infections.
There is wide variation in the extent to which retesting occurs, and this important aspect of care was more likely to be accessed by European females than other groups. High rates of reinfection were observed among those who are retested – most likely reflecting gaps in the treatment of sexual partners. When someone is diagnosed with chlamydia or gonorrhoea, they should be advised to talk to recent sexual partners so they can get checked and treated. A combination of factors at patient, provider and health system-levels are likely to be impacting on whether partners are notified, and whether or not those partners can access care for testing and treatment.
Further research is urgently needed to identify service-level changes that enable equitable access to care, and that effectively support the routine delivery of best practice care across the STI management pathway.
Research team
Dr Sally Rose, Sue Garrett, Professor Sue Pullon (Department of Primary Health Care and General Practice, University of Otago, Wellington), Associate Professor James Stanley (Biostatistical Group, University of Otago, Wellington).
Acknowledgements
We wish to thank the Hawkes Bay Medical Research Foundation for funding this work. We also acknowledge the clinicians in Hawkes Bay, Tairāwhiti, MidCentral and Whanganui regions for generously giving their time to participate in key informant interviews. Thanks to staff at Southern Community Laboratories and MedLab Central for the provision of STI testing data, and the Ministry of Health for the provision of ethnicity and NZDeprivation data.
Ethical approval: This study was approved by the Central Health and Disability Ethics Committee on 01 August 2017 (Ref 17/CEN/128)
